These diseases are syndromes where congenital renal tubular dysfunction causes hypokalemia and metabolic
alkalosis, as well as their associated clinical symptoms.
Bartter syndrome usually occurs from the neonatal period to infancy, whereas Gitelman syndrome usually
occurs from infancy to school age, but some patients remain asymptomatic for life.
Kidney tubules reabsorb water and electrolytes essential for the body from the primary urine, which is the
source of the urine. In Bartter/Gitelman syndromes, congenital dysfunction of the kidney tubules cause a
decrease in blood electrolytes, and symptoms, including a feeling of weakness, muscular symptoms, and/or
polydipsia/polyuria, appear, especially due to hypokalemia. Growth disorders such as short stature may also
occur. Furthermore, some patients progress to end-stage kidney disease. Hearing loss is also observed in some
types.
Other than the above, so-called unidentified clinical symptoms (fatigue, headache, dizziness, and marked
fatigue especially when suffering from a cold) are present in many patients, but some patients are not aware
that these symptoms are due to the disease.
Currently, there is no specific treatment. Treatment is mainly symptomatic such as electrolyte supplementation. However, nonsteroidal anti-inflammatory agents are sometimes effective, and so these medicines are recommended when electrolyte supplementation alone does not improve symptoms.
According to a large-scale survey on the number of patients receiving medical care in Japan, the estimated number of patients as of 2017 was 550. However, given that this disease cannot be diagnosed without a blood test, the potential number of undiagnosed patients seems to be large.
Bartter syndrome and Gitelman syndromes are both known to be caused by genetic abnormalities.
The mode of inheritance for these diseases is mostly autosomal recessive. This means that if, by chance, parents are both asymptomatic carriers of a genetic abnormality, each child has a 1 in 4 chance of developing the disease. It is rare that a patient passes the disease on to his/her children.
Some patients with Bartter syndrome progress to end-stage kidney disease. In some patients of these
diseases, growth disorder such as short stature and hearing loss are also present.
Gitelman syndrome is milder in severity than Bartter syndrome, and has a favorable kidney prognosis.
However, as described above, both diseases may be associated with unidentified clinical symptoms such as
fatigue, which affect everyday life

The kidney is an organ that excretes excess water and unnecessary waste in the blood into the urine. By
this function, the blood in the body is always kept clean, and water volume and electrolyte levels in the
body are regulated to be constant. This may sound easy when described in words, but the process involves
very complicated tasks as below:
1. A large volume of blood is perfused to the kidneys via the arteries (Figure 1).
2. Excess water and unnecessary waste in the blood are discharged from the kidney glomerulus into kidney
tubules (Figure 2).
3. To balance the electrolytes in the blood, electrolyte exchange is performed between the urine in the
kidney tubules and the blood in the capillary blood vessels (Figure 2).
4. Then, the urine flows from the kidney tubules into the ureters and bladder (Figure 1).
5. The purified, clean blood flows into the veins (Figure 1).
This disease is caused by mutations in the gene that encodes the transporter that transports the electrolytes, sodium and chloride from the urine into the capillary blood vessels in kidney tubules described above. Because of the transporter dysfunction, a large amount of sodium leaks into the urine. To stop sodium necessary for the body from continuing to leak into the urine, potassium and magnesium, which are both cations like sodium, also leak into the urine in large quantities. Consequently, blood potassium and magnesium decrease, leading to hypokalemia and hypomagnesemia.
Due to hypomagnesemia and hypokalemia, symptoms such as getting tired easily, numbness in limbs, cramps
in limbs, muscular pain, and headache appear. In addition, because sodium leaks into the urine in large
quantities, as described above, urine osmotic pressure increases, and as a result, a lot of water also
leaks into the urine. Because of this, patients with this disease typically drink a lot and urinate a lot
(polydipsia, polyuria). In particular, although urinary output should normally decrease during the night,
patients with Gitelman syndrome frequently urinate also during the night and may have nocturnal enuresis
or wake up to go to the toilet once or twice during the night. Furthermore, patients get exhausted to an
unusual extent when suffering from a common cold and may even require transfusion and/or hospitalization.
As another feature of this disease, patients are often short-statured. On the other hand, some patients
remain asymptomatic for life.
Patients with this disease typically prefer sodium-rich meals to supplement sodium, which leaks into the
urine in large quantities. During childhood, many some patients may drink soy sauce or lick salt. This is
not absolutely recommended, but sodium-rich foods need to be provided to some extent.
As a very rare complication, long QT syndrome, which may lead to sudden death due to arrhythmia, has been
reported, but this arrhythmia disappears in most cases by appropriately supplementing electrolytes.
To improve all symptoms, treatment is necessary to maintain potassium and magnesium levels at a certain
level or higher.
The most important treatment is the supplementation of potassium and magnesium. By this, blood potassium and magnesium levels increase. However, even after this treatment, various symptoms may remain. Also, this treatment is not effective for bedwetting and polyuria at all. If these symptoms are present to the extent that everyday life is affected, oral nonsteroidal anti-inflammatory agents (brand name: Infree, Inteban, etc. Inteban is not on the market in Japan as of 2019) are used. Currently, these drugs are considered most effective, but as long-term use may cause kidney side effects, caution should be taken. Patients can visit a pediatric or internal medicine clinic, but as Gitelman syndrome is relatively rare, most physicians have no clinical experience of treating this disease. Therefore, even if the patient complains of symptoms associated with Gitelman syndrome, the physician may not able to make the correct diagnosis or judgment sometimes.
Gitelman syndrome is typically considered a mild disease, but symptoms, including getting tired easily,
become obvious with age and may affect everyday life; for example, it may be difficult to continue working
because of these symptoms. Oral use of above-mentioned nonsteroidal anti-inflammatory agents may mitigate
the symptoms to some extent, and so patients are advised to consult with a doctor.
In some patients, kidney function may slowly deteriorate, and there have also been reports of patients
requiring dialysis. Furthermore, as described above, if the potassium level is not controlled, long QT
syndrome may cause arrhythmia and sudden death, although this is very rare.
Most symptoms associated with Gitelman syndrome are unidentified clinical symptoms, which are often observed in adolescence (e.g., feeling weary, having a headache, and getting tired easily). Therefore, these symptoms may be considered by others to be just a “matter of feeling,” and so more understanding is necessary about this. In addition, there are some patients who are deeply troubled because, in spite of being in adolescence, they have bedwetting episodes every night. General medicines for nocturnal enuresis have little effect. People around patients need to understand about this problem. Furthermore, when suffering from a cold (e.g., influenza), patients with this syndrome typically get exhausted and feel their symptoms more severe to an extent that appears exaggerated. Therefore, when they have a cold, please try to understand their condition and let them have a good rest.
As patients with Gitelman syndrome often present with so-called unidentified clinical symptoms, including fatigue, dizziness, and muscle weakness, their condition is sometimes mistaken for a psychiatric disease. On top of the fatigue patients usually have, they experience more severe fatigue and a reduced activity when they have a cold. Common symptoms in adult patients with Gitelman syndrome and their frequencies are as follows: salt craving (liking salty foods, 90%), myospasm (cramp, 84%), fatigue (82%), dizziness (80%), night pollakisuria (80%), thirst (76%), and muscle weakness (70%) (cited from Cruz et al., KidneyInt 2001). Most of these symptoms are considered to be associated with the disease. It is necessary to create an environment to help both patients and people around them have a deeper understanding of the symptoms of Gitelman syndrome.
Brochure about Gitelman syndrome
Download
Diagnostic criteria for Bartter syndrome/Gitelman syndrome
(developed by research group)
Essential criteria
1. Hypokalemia (serum potassium: ≤ 3.5 mEq/L)
2. Metabolic alkalosis (blood gas analysis [HCO3-]: ≥ 25 mEq/L)
Referential criteria
1. Increase in plasma renin activity
2. Increase in plasma aldosterone level
3. Normal blood pressure or hypotension
4. Polyhydramnios, premature delivery, low birth weight, nephrocalcinosis, and hypercalciuria (Type 1 or
Type 2 Bartter syndrome is strongly suspected)
5. Polyhydramnios, premature delivery, low birth weight, and hearing loss (Type 4 Bartter syndrome is
strongly suspected)
6. Either hypomagnesemia or hypocalciuria alone or both (Type 3 Bartter syndrome or Gitelman syndrome is
strongly suspected)
* If criteria 4 to 6 above are not met, the possibility of Type 3 Bartter syndrome should be considered.
Differential diagnosis
The following diseases are excluded:
1.Secondary causes: use of diuretics/laxatives, severe hyperemesis gravidarum, anorexia nervosa, habitual
vomiting, excessive dieting, and alcoholic intoxication may cause so-called pseudo-Bartter/Gitelman
syndromes.
2.Other hereditary diseases: hypoplastic kidney, nephronophthisis, Dent disease, mitochondrial disease,
congenital renal tubular diseases such as autosomal dominant hypocalcemia (ADH), cystic fibrosis, and
congenital chloridorrhea. In these diseases, the clinical condition may be similar to that of Bartter
syndrome, and in such a case, it can be very difficult to make the differential diagnosis from Bartter
syndrome. In particular, it has been reported that the onset of ADH due to an activating mutation of the
calcium-sensing receptor (CaSR) gene (CASR) leads to a clinical condition similar to that of Bartter
syndrome, and this condition is sometimes categorized into Type 5 Bartter syndrome. However, even if there
is a mutation in the CASR gene, Bartter syndrome-like symptoms rarely appear, and so this condition is not
considered to be a subtype of Bartter syndrome in the diagnostic criteria.
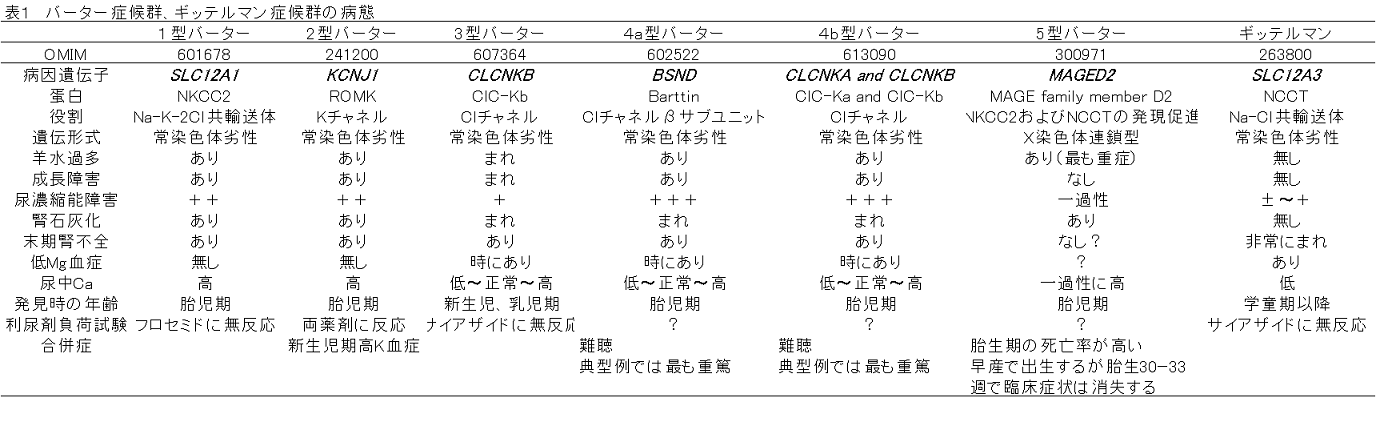
Genetic testing
Genetic diagnosis is made with reference to Table 1. Recently, all disease types can be exhaustively
analyzed by an analysis using a next-generation sequencer.
Cases with a “definite” diagnosis as defined below.
Definite: Both essential criteria are met, all differential diagnoses are excluded, and the causative
genetic mutation is identified by genetic diagnosis.
Probable: Both essential criteria are met, all differential diagnoses are excluded, and although the
causative genetic mutation is not identified by genetic diagnosis (genetic diagnosis has not been performed
or has been performed without identifying the causative genetic mutation), three of the referential criteria
are met.