It is a disease characterized by protein, which does not normally leak from the blood, going out into the urine in large quantities, leading to a decrease in serum protein level (hypoproteinemia). Due to this, various symptoms such as swelling (edema), dyslipidemia, abnormalities in the coagulation-fibrinolytic system (increased tendency for blood clotting), and immune abnormalities (susceptibility to bacterial infection) appear. Nephrotic syndrome that develops within 3 months after birth is categorized as congenital nephrotic syndrome (CNS), while that which develops within 1 year after birth is categorized as infantile nephrotic syndrome (INS). The representative type of congenital nephrotic syndrome is congenital nephrotic syndrome of the Finnish type (CNF).
If the patient develops nephrotic syndrome within 3 months after birth, and the following
clinical symptoms and laboratory findings are observed, a provisional diagnosis is made. Then,
kidney tissue examination and gene testing are performed as far as possible, and based on a
comprehensive evaluation of the results, the diagnosis is confirmed.

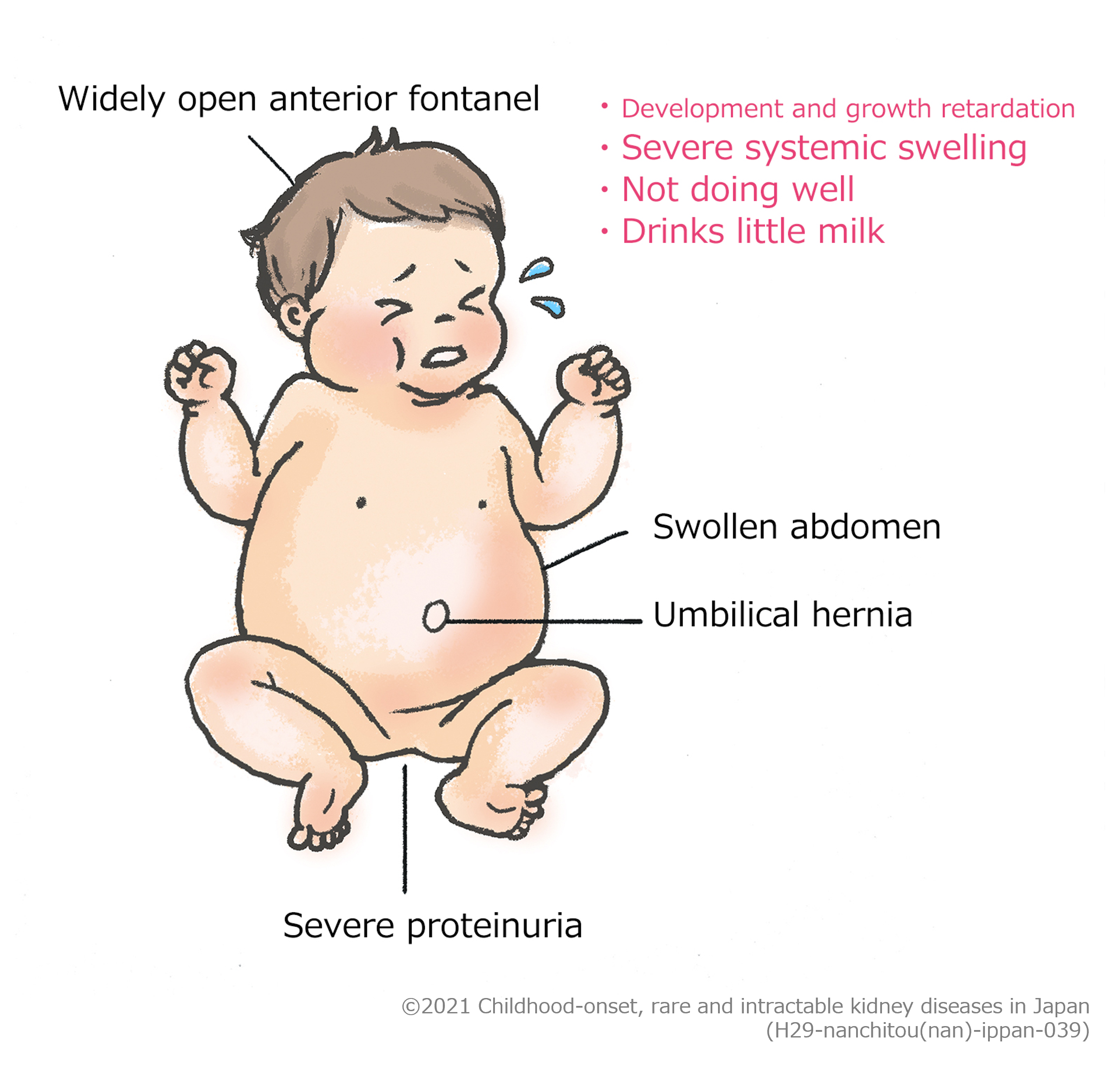
Abnormalities in the amniotic fluid components are observed due to a large amount of protein leak into the urine, which starts from when the baby is still in the uterus of the mother. In addition, it is known that a giant placenta weighing ≥ 25% of the weight of the baby is generated. However, the diagnosis is rarely made during pregnancy and is instead generally made after birth. A lot of patients present with nephrotic syndrome (severe proteinuria, hypoalbuminemia) from just after birth, with symptoms such as severe systemic swelling, ascites, and widely open anterior fontanel. Moreover, mild abnormalities may be present in the functions of the central nerves and heart.
Unlike pediatric idiopathic nephrotic syndrome, no drug therapy is available for congenital nephrotic syndrome of the Finnish type, and so renal transplantation becomes necessary eventually. Initially, conservative treatment for severe nephrotic condition is performed. Because it is necessary to regularly supplement albumin by infusion and administer diuretics to manage swelling, the length of hospital stay is prolonged. If daily albumin supplementation by infusion is required for a long period of time, infusion is performed via a long-term indwelling catheter placed in the central vein, which is a thick blood vessel near the heart. Captopril and indomethacin may be used for treatment aimed at decreasing urine protein. It may also be necessary to feed milk via a tube inserted into the nose to give sufficient nutrition. Since various components other than protein leak into the urine, vitamin preparations including vitamin D, minerals, thyroid hormone, etc. should also be supplemented, as appropriate. In addition, it is important to prevent thrombosis and to treat infection quickly for the management of complications. The swelling control is often difficult even with the above-mentioned treatment, therefore, the kidney is generally removed to prevent protein leak. In Japan, there are many patients in whom their condition becomes manageable by removing one of the kidneys (unilateral nephrectomy). Depending on the condition, however, both kidneys may be removed.

In Japan, according to the survey as of April 1, 2015, the prevalence of congenital nephrotic syndrome of the Finnish type is reported to be 0.30 in 100,000 births. In Finland, the frequency is higher and is estimated to be about 1 in 8000 births.
TheNPHS1gene is reported to be the responsible gene for congenital nephrotic syndrome of the Finnish type, but the gene is not detected in some patients. In cases of congenital nephrotic syndrome other than those of the Finnish type, abnormalities in a gene other than the NPHS1gene are observed.
In cases of abnormalities in theNPHS1gene, the mode of inheritance is autosomal recessive.
Congenital nephrotic syndrome of the Finnish type used to have a high mortality rate and a poor prognosis in the past, but since the introduction of a treatment strategy that involves removal of one or both kidneys, followed by peritoneal dialysis (PD) and then kidney transplantation, a better vital prognosis as well as improvement in growth impairment and psychomotor retardation are becoming achievable.
Highly intensive management may be required from the neonatal period, and then later, the patient may need to be treated at an institution capable of performing pediatric peritoneal dialysis and undergo kidney transplantation at an institution capable of providing such intervention. Therefore, treatment should preferably be given at a university hospital where pediatric kidney specialists are available or a medical institution that can cooperate closely with a pediatric hospital.
According to a nationwide questionnaire survey as of April 1, 2015 in Japan, 25 of 33 patients with congenital nephrotic syndrome of the Finnish type under the age of 16 had undergone the surgical removal of one kidney (unilateral nephrectomy), with the median time after birth being 13 months (3 months to 96 months).
Symptoms of nephrotic syndrome appear just after birth, and inpatient treatment is required in many cases due to the necessity of treatment for severe systemic swelling. The patient needs to stay in the hospital until the swelling is relieved, and the administration of albumin by infusion becomes unnecessary after the removal of one kidney and/or treatment with drugs to reduce urinary protein. Generally, about 6 months to 1-year hospitalization is required, but the duration of hospital stay varies depending on symptoms and institutions. If the patient has an infection due to bacteria, etc. during the treatment, the duration of hospitalization is prolonged.
Some can drink milk by mouth, but many cannot orally consume a sufficient amount of milk as nutrition because they have little appetite due to a swollen abdomen full of water or a swollen intestine caused by severe systemic swelling. Consequently, for these babies, it becomes necessary to insert a tube through the nose to give milk directly to the stomach or duodenum or to place a tube directly into the stomach (gastrostomy) to administer sufficient nutrition.
During the period when treatment for severe systemic swelling is required, treatment by infusion is given to supplement albumin. Albumin may need to be supplemented every day. In addition, various components leaking from the body need to be supplemented by infusion or orally. After protein leaking from the kidneys is reduced by the removal of one kidney, outpatient treatment is continued to supplement necessary components with oral medications.